Abstract
Introduction: Mantle cell lymphoma (MCL) is known to affect elderly patients with a median age of diagnosis of 68 years. While autologous stem cell transplantation (ASCT) in CR1 is an established consolidation treatment for younger patients, its role in the elderly is not clear.
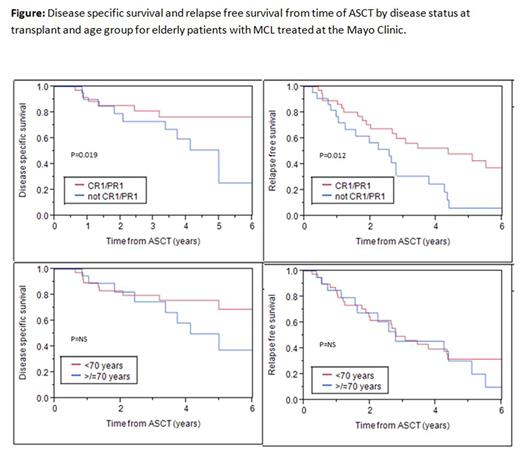
Methods: We performed a retrospective chart review of patients who underwent autologous stem cell transplantation at the age of 65 years or older at the Mayo Clinic for the treatment of MCL. Patients in CR1 and PR1 were both considered to be in first response as PET scans were not done for all patients. Outcomes were measured as time from ASCT until relapse (relapse free survival, RFS) and until death due to any cause (overall survival, OS).Due to possible competing causes of death in the older patients, disease specific survival (DSS) was measured as time from ASCT until death due to MCL. Survival analysis was done by the Kaplan Meier method using the log rank test between groups.
Results: 63 elderly patients (≥65 years of age) underwent high dose chemotherapy (BEAM/BEAC) followed by ASCT for a diagnosis of MCL at the Mayo Clinic sites [46 at Rochester (1998-2016), 12 at Florida (1999-2016) and 5 at Arizona (2008-2016)]. Median age at diagnosis was 67 years (range 53-74.5 years) and at ASCT was 68 years (range 65-77.4 years). 22 (34.9%) patients were ≥70 years at the time of ASCT. The majority of patients were Caucasian (62, 98.4%) and males (45, 71.4%). Only 12 (19%) patients received cytarabine based induction. Most patients (38, 60.3%) received R-CHOP as their first line therapy. 38 (60.3%) patients had only one line of therapy prior to ASCT. At the time of ASCT, 33 patients (52.4%) were in CR1, 7 (11.1%) in PR1, 9 (14.3%) in CR2, 5 (7.9%) in PR2, 6 (9.5%) in CR/PR 3 or beyond and 3 (4.8%) in relapse. Median time to ASCT from diagnosis was 0.7 years (range 0.4- 15.7 years, IQR 0.5-2.7 years).
At the D+100 post-ASCT evaluation, 2 patients were in PR and 1 patient had relapsed while all others (96.2%) were in CR. At a median follow-up of 2.8 years after ASCT (range 0.24-12.1 years), 35 patients had relapsed while 28 remained in post-ASCT remission. 26 patients had died- 18 from MCL, 3 from secondary neoplasms (2 from myelodysplastic syndrome and 1 from metastatic prostate cancer), 1 due to GVHD from subsequent allogeneic SCT, 1 from an accident and 3 due to unknown causes. There was no ASCT related mortality.
Median OS from time of diagnosis was 7.9 years and from time of ASCT was 5 years. Median DSS was 10.8 years from diagnosis and 7.6 years from ASCT. Median RFS post-ASCT was 3.2 years.
Survival differed significantly with disease status at the time of ASCT. At 3 years, RFS was 60% vs. 30.9% [P=0.012]; DSS was 81.4% vs 73.2% [P=0.019] and OS was 73.8% vs 69.6% [P=0.012] for those in CR1/PR1 versus those not in first response at the time of ASCT (figure). Post-ASCT survival (OS, DSS, RFS) did not differ by sex or age at ASCT (<70 versus ≥70 years).
Among the 40 patients that underwent ASCT in CR1/PR1, only 3 received more than one line of therapy prior to transplant. The DSS and RFS were not significantly different whether RCHOP or ARAC based regimens were used as induction.
Conclusions: Selected patients older than 65 years of age can safely undergo ASCT for MCL and chronological age alone should not be the reason for exclusion from ASCT. ASCT when performed in first response (CR1/PR1) is more effective than at more advanced disease or relapse even in older patients.
Reeder: Bristol-Myers Squibb: Research Funding; Celgene: Research Funding; Novartis: Research Funding; Millennium: Research Funding; Affimed: Research Funding. Ansell: Celldex: Research Funding; Merck: Research Funding; Affimed: Research Funding; Seattle Genetics: Research Funding; Bristol-Myers Squibb: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal